Why is this subject, “Not In Vain, A Promise Kept,” important in the world?
Today patient advocacy is more important than it was 12 years ago when my Mom was diagnosed with ovarian cancer. In my opinion, healthcare has gotten worse, not better. If you or one of your loved ones becomes sick while you are not on the hospital payroll, you, by default, become part of the patient team. Whether you sign up for it or not, it is reality. It is your job, and if you want to achieve the best outcome, it is absolutely in the patient’s best interest.
The pandemic has also significantly impacted healthcare, doctor-patient relationships, health insurance, government overreach, pharmaceutical companies, and individual health autonomy and freedoms.
Doctors were fighting a virus that plagued many without appropriate resources, direction, approved treatment approaches, and government mandates for over two years. They were put into environments that were unsafe for them but under extreme stress and pressure. Many patients that entered hospitals with Covid-19 never got out. While there are questions about the actual number of those who died from Covid-19, the WHO has the number globally at roughly 6.8 million. During 2020 and much of 2021, a lot of preventative screening, non-emergency surgeries, annual physicals, routine labs, radiology tests, exploratory surgeries, etc., were put off due to the surge in Covid and the need to reduce the spread; therefore, eliminating “normal” annual care.
Due to the inability to access care, many people who may have caught the disease at an earlier stage are presenting with more advanced disease increasing the complexity and resources needed to treat and potentially cure and maintain effectively. Healthcare staff are burned out mentally and physically. I was a patient at the end of 2020 for a rare stomach issue. I went to a local emergency room in extreme pain.
I was there for seven hours, had an emergency endoscopy, and was told that nothing was wrong with me, and I was being discharged. They were not swamped, and I was in no condition to go home. I was in so much pain; if I could have reached my phone, I would have called 911. At that moment, I found out what a code gray was in a hospital. A code gray means a “combative patient.” I was not combative; when I found out I was being discharged, I reiterated that I was not “ok” and was in extreme pain, vomiting, and, quite frankly, dying. Thankfully after my discharge papers were drawn up for signature and my vitals and IVs were disconnected, I got up to use the bathroom and passed out. When I woke up, the same nurse that deemed me a code gray was with another nurse flooding my body with fluids because my blood pressure was 70/30 and I was severely tachycardic. A hospitalist was called to the bedside, took over the case, and had to rewrite and update my entire file. He ordered labs, and I was severely anemic, and my CBC had many irregularities. They suspected a GI bleed, and I was admitted. Remember that this was 2020, and no visitors were allowed in the ED or visit an inpatient.
I was alone, in extreme pain, and scared.
He ordered a cat scan the following day, and within an hour of receiving the results, I was being run down the hallway into the operating room by a trauma surgeon who ultimately saved my life. I had gastric volvulus. It is rare yet very fatal. My stomach flipped over and disconnected from my spleen. I required 4 liters of blood and woke up two days later in the ICU.
I believe my case was not unique and a real example of a tired, overworked, understaffed, and frankly dangerous physician assistant that failed to do the basics of most emergency room visits, like labs, except for a covid-19 test. If I had not passed out, I would have died within hours at home. My example is and continues to be a problem.
While it sounds cliché, healthcare is sick, both mentally and physically. I absolutely have empathy and can’t imagine the trauma that doctors and nurses went through for two-plus years, but there is no room for gross negligence. That is how people die, and I almost did at home with my husband and ten-year-old son if I was not lucky enough to pass out before discharge.
What is the pressing issue right, and how are you addressing it?
The healthcare industry is facing several pressing issues today, from the high cost of healthcare to staffing shortages, burnout, access to care, and availability to very long wait times in scheduling.
One of the most significant issues is the rising cost of health care. According to a survey by the Kaiser Family Foundation, 35% of Americans have struggled with medical or dental bills they are paying off over time. “The cost of care can also lead some adults to skip or delay seeking services. One-third of adults say they or another family member living in their household has not gotten a medical test or treatment that was recommended by a doctor in the past year because of the cost, while about four in ten (43%) report that they or a family member in their household has put off or postponed needed health care due to cost.”
Another major issue in healthcare today is the lack of interoperability between systems. This can lead to inefficient clinical workflows and personnel shortages, ultimately affecting patient care. In a post-pandemic world, many medical facilities have been plagued with staff shortages, terminations, loss of talent through early retirement, budget issues, and what I call an overall total system hangover.
I just lost my Dad to complications of CHF in the last three weeks of 2022. He was hospitalized twice. From pure observation and without bias, I see a stressed system. I see an understaffed, under-supervised workflow. I see shift changes that take three hours and patients that wait for medications that are readily available for hours. The high-stress, low-motivation environment is a mental breeding ground for patient mistakes and errors. There are many part-time or traveling nurses who, in reality, have no skin in the game. I don’t care if you are the most clinically savvy and skilled nurse available, if you are on an oncology floor on Monday, backing up in Cardiology on Tuesday, or on Med/Surg the rest of the week, how good are you at your job and the unique role requirements for the patient population and how much do you care about your job performance? You are still getting paid, no matter your performance. In fact, you are probably getting paid more than your peer nurses that pull a paycheck from the hospital facility, so there is normal friction.
In my Dad’s scenario, there were many errors. There was miscommunication and failure to treat effectively and timely. He ultimately died on December 30th. While his prognosis was terminal, he suffered due to orders not being fulfilled and doctors not being on the same page as what was agreed upon in the patient record. As his daughter and advocate, I was there every day all day and was at the mercy of those in charge. While I advocated consistently and thoroughly, I still fell short in the end, and he suffered.
What am I doing about it? I documented everything. I downloaded every patient interaction, conversation, lab, x-ray result, used the electronic patient portal, visited at the beginning of visiting hours to try and catch doctors making rounds, asked for business cards, and wrote a letter to the person in charge of the facility. My goal is to educate this person on what is happening in his facilities and make changes.
I never thought I would be in this position again, but here I am. I will not give up and will forever share my experiences and learnings with others to try and prevent others from going through preventable suffering, medical errors, and complications. I wrote “Not in Vain, A Promise Kept” about my Mom’s journey with cancer and my family’s experiences; I didn’t plan on writing a book about my Dad, but it is not off the table.
Melissa Mullamphy Biography
What is your background in this subject?
The subject of patient advocacy is a tricky one.
For me, it is both experience and education. I have a masters in counseling psychology and have worked in various mental health hospitals and facilities. I am an avid student. I read and researched a lot. To be an effective patient advocate, you must try and understand illness, diagnosis, testing, medications, treatments, alternatives, trends, statistics, medical roles, medical specialties, healthcare facilities, patient rights, wellness, and preventatives; the list is endless. While the internet is a great place to research, you will never replace your doctor, but it is in your best interest to be armed with information.
The more educated a patient and patient advocate are about an illness, the better the outcome will likely be. One of my Mom’s doctors once told me doctors told me to “stay off of the internet” when she was having deadly side effects from chemotherapy. I googled the drug, and my Mom had every symptom of toxicity except coma and death, and he assured us that she “was fine.” Three awful days later, he came into my Mom’s hospital room and told me I was right and that she was toxic. I did not take pleasure in being right, BUT I should have trusted my gut and not allowed them to proceed with three additional daily rounds of poison. Being toxic from chemotherapy caused her to lose two weeks of her life, hallucinating and suffering. The priest was called into her room three times because she was dying from being poisoned. While her prognosis at this time was guarded, I firmly believe it was at this junction that she lost all hope and fight that she had left.
What is something that most people don’t know about you?
My husband is my high school sweetheart, and we had our miracle baby at the age of 39. We have been together since 1985. We grew up together, he served in the United States Marine Corps and deployed overseas, and I have lived in both New York State and North Carolina. I worked in the reinsurance industry for just shy of twenty years for General Re, which is owned by Warren Buffet. While I did not go to college to work in the insurance or reinsurance industry, I learned from the best and found a niche. I had many male and female mentors who now run companies and board rooms. I was fortunate to find such an opportunity and learn and work with some of the best in the business. They took a chance on a young New Yorker with an attitude, unpolished, sometimes a little too direct and inexperienced girl from the suburbs of NYC, and turned her into a corporate leader with unlimited potential. Part of my role was as a domestic operations manager, and I traveled a lot in the US and Canada. I keep in touch with many of my former colleagues and bosses today, as they are like family. I would not change a thing.
What are your passions outside of your career?
A blue-collar family raised me. The home I grew up in was roughly 900 square feet, and my sister and I shared a room until she moved out. We had bunk beds. My parents worked and taught my sister and me how to be self-sufficient, independent, and have a good work ethic. My Mom was a great artist, and my Dad kept our lawn meticulously; even up until this last Fall, he was picking up leaves in his yard daily. He was the “Edward Scissor Hands” of landscaping. I spent most of my adult life inside an office or a classroom, so I like to be outside and try to keep my yard in good shape and plant flowers and have managed to get my son interested in doing the same. So, while I do not have “Edward ScissorHands” skills, I do enjoy planting flowers and landscaping. We also have five large dogs that keep us very busy. I also enjoy spending time with my family. Time is so precious, so it is important to make memories.
Are there any social causes that you believe in and support?
I am and have always been a big supporter of our veterans. Perhaps it is because I am married to one, but I feel that we always need to look within to see how we can improve how we treat them, what we offer them, what they are entitled to, and how to help them with battle the wounds of war that you do not see such as mental illness, veteran suicide, PTSD and TBI. In my opinion, we are currently in crisis mode with mental illness, suicide, homelessness, and addictions, and we must do better. I have supported Wounded Warrior Project for many years, led non-profit events for veterans, and continue to spread awareness, support, and volunteer for sponsoring, donating, and helping those I can using my platform.
What is next for you?
Right now, my Dad is gone three months, March 30th. While I continue to grieve his loss, I am also seeking accountability from the hospital facility that dropped the ball with his care. I blog daily about current healthcare and patient advocacy events and offer advice and suggestions on finding your voice and actively participating in healthcare as a patient or caregiver. I have considered writing a couple more books in the future, particularly after what I just went through with my Dad and I was there. What happens to those who have nobody? I’ll tell you, meet my neighbor, Mr. Paul Swing: https://www.melissamullamphy.com/post/it-s-not-ok-to-die-alone-it-s-not-ok-to-let-a-human-being-suffer.
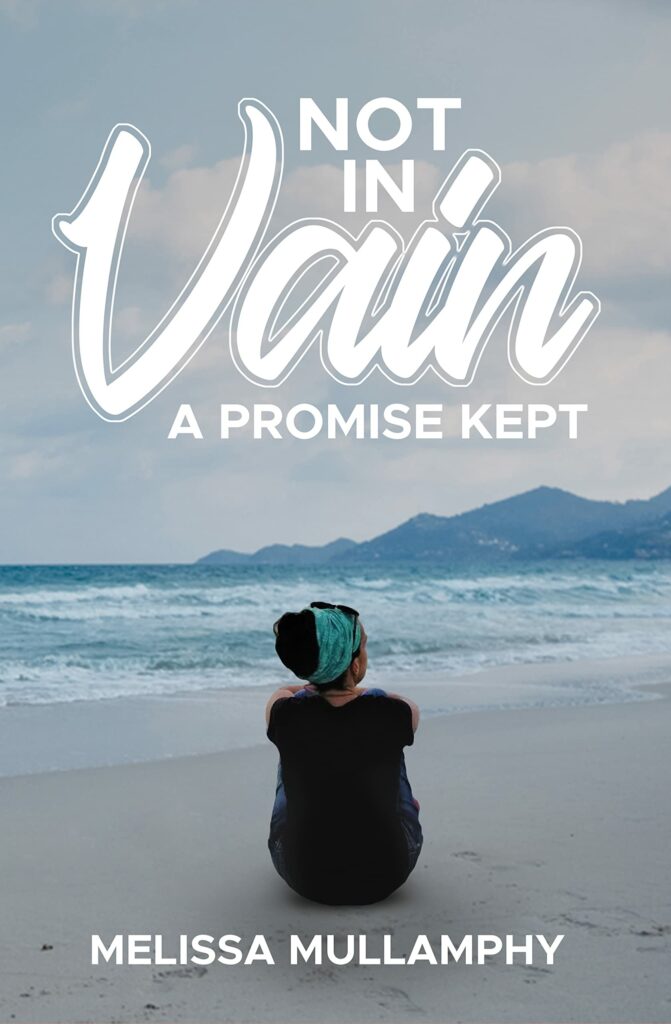
Not In Vain A Promise Kept
Tell me about your book.
An unflinching chronicle of loss that takes a hard look at the state of medical care in the United States. — Kirkus
Over the course of this book, the descriptions of the author’s mother’s worsening symptoms are chilling, but the most disturbing parts are those that recount the family’s struggles with the healthcare system. In one case, for instance, Mullamphy writes that she suspected that her mother, who suffered from constant, severe nausea, had been poisoned by excessive chemotherapy, which an oncologist later confirmed. However, what sets the author’s work apart from other memoirs of grief are her expressions of anger a decade after her mother’s passing and how accessible she makes these emotions to the reader. She tells of doggedly pursuing answers while dealing with seemingly apathetic doctors, and her layman’s translations of medical jargon even offer occasional lighter moments: “What the hell is platelet apheresis? It is a big machine similar to dialysis…like a rinse cycle, but it removes extra junk that can kill you instead of cleaning clothes.” The author writes that she worked on this book for a decade as a promise to her mother, expressed in the title. In it, she’s candid about the ugly parts of her own grieving process, including accounts of her worsening performance at a corporate reinsurance company and the seizures she endured, partly due to stress; she was eventually diagnosed with a neurocognitive disorder in 2013. Mullamphy’s impressions of her mother’s medical care oscillate throughout the work but may be summed up with the dictum that one shouldn’t blindly trust medical staff “because the human error happens.” She also effectively stresses the importance of “watching over your loved ones and advocating for them when they cannot or won’t.”
Where can people buy the book?
My goal in writing this book is to keep my promise to my Mom one late night in her hospital room while she was suffering yet another complication from cancer, to share her story so others don’t go through what she and my family went through.
You can have input, control, and make a difference in your loved one’s healthcare.
You can be their best advocate.
Dentist transforms lives with one smile, globally and locally(Opens in a new browser tab)
You will learn lessons and tips to help you support your loved ones through example, help you find your voice, and understand your rights in a very complicated and imperfect healthcare system.
FOR MORE INFORMATION VISIT: melissamullamphy.com
FOR MORE INFO ON THE BOOK VISIT: Not In Vain, A Promise Kept | Melissa Mullamphy